Written by Taylor Hart a Childhood Trauma Specialist & Alyse Bone an ADHD Specialist
All opinions expressed in this blog are solely those of the authors and do not reflect the opinions of Dandelion Family Counseling, PLLC.
Parents are constantly encouraged to be mindful of their child’s behavior. This often leads to a natural tendency where a parent may compare challenging behaviors to those of Damian’s constant fidgeting or Rebecca’s tendency to shut down when given instructions. These traits of Damian and Rebecca are common when we think of the diagnosis, ADHD. However, there are many cases where ADHD can present with symptoms similar to other diagnoses (sometimes, it is not necessary to focus on a diagnosis at all). That’s right – there are overlaps between ADHD and other concerns! This article will focus on building awareness in parents and significant caregivers about the basics of ADHD and trauma for children, including their similarities and differences.
Defining Childhood ADHD:
Attention Deficit Hyperactivity Disorder, or better known as ADHD, is a developmental disorder, which means that a person is born with that impacts a child’s executive functioning abilities (take a look at a few examples below).
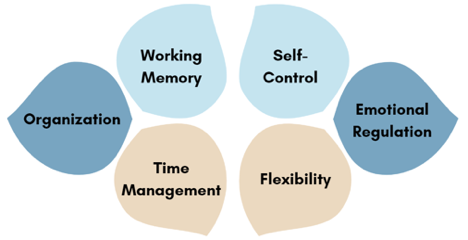
A person can predominantly be inattentive where their experiences are more related to difficulties with attention or hyperfocus. On the other hand, a person can be hyperactive/impulsive meaning their experiences are more related to that kiddo that you would see bouncing off the walls and cannot keep still. Lastly, a kiddo can have both! While the main symptoms associated with ADHD are related to executive functioning, the sub-symptoms are important to acknowledge as well. These symptoms present themselves in most children due to the executive functioning challenges and include: Anxiety, depression, social concerns, low self esteem, low self confidence, school concerns, trauma, and family dysfunction.
Defining Childhood Trauma:
Trauma, a complex term, is one’s experience of a distressing event, tragedy, or period of time that impacts our emotional state and alters how we function. This knowledge is a big deal when we prioritize helping children develop and function throughout childhood, because this fact gives us insight on a barrier to learning. When a child’s brain captures a high level of stress without helpful support from a trusted caregiver, it causes the body to move into a state of survival for a prolonged period of time. This high level of stress is naturally harmful to many areas of the brain, causing extreme difficulty with remembering instructions, learning, engaging with others, and having a positive view of themselves to name a few. Trauma can occur when a child is directly involved in a distressing experience, or has witnessed a distressing experience happen to someone or something else. This means that it can be traumatic for a child to endure a chronic illness such as cancer, just as it can be traumatic for a child to witness a sibling’s experience of a chronic illness.

Symptoms of Childhood Trauma:
Trauma can impact children differently than adults; children may not show symptoms of trauma right after the event has occurred and may not be able to process their experience right away. Three common misconceptions are that (1) The child will get over the trauma when we choose not to bring it up and symptoms will get better, (2) The child will forget the trauma as they get older and symptoms will get better, and (3) If symptoms are not noticeable then the child is just fine. The hard truth is that trauma is a serious matter impacting the growth of children and symptoms are not always noticeable without an assessment. Although we may forget certain details overtime, our bodies store unforgettable felt memories that can create long-term symptoms well into adulthood. When parents or significant caregivers avoid supporting a child through a traumatic experience, it is often with the hope to prevent sadness and disappointment. However, doing so actually delays the growth of a child and prolongs the unpleasant feelings they are already carrying.
Since every child is different, symptoms will also look different from child to child. In fact, the symptoms of experiencing a traumatic event can look quite similar to the symptoms of ADHD. The image below shares a few:
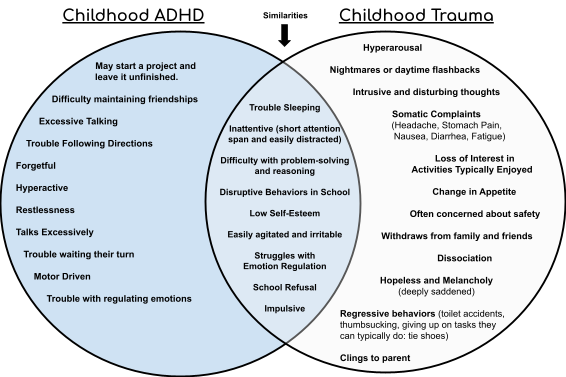
The diagram above displays the similarities and differences between childhood ADHD and Trauma. When we understand the root cause it helps us discover how to connect with the child and support their behavior. There is also a fundamental difference between these two diagnoses which correlates with the child’s development and their experience. Trauma causes symptoms that may develop overtime, and are often seen through a child’s decisions, interests, and actions; this is similar to ways that children with ADHD may communicate. Consider whether the child creates art images that appear aggressive, avoids sharing about their feelings, has begun to isolate from classmates during the school day, or focuses only on tasks they do well to mask where they are struggling.
Children experience traumatic events in their life that can rewire their brain and this impacts how they perceive the world. ADHD and trauma can display as developmental delays. Trauma is due to the onset of a distressing experience while ADHD is a neurodevelopmental disorder. Children are able to seek treatment to improve their symptoms no matter the diagnosis. Every child is different and this means that treatment along with the outcome will also differ. It is important to seek a provider who understands child development and has experience with both ADHD and trauma. There is a distinction between ADHD and trauma, but children can be diagnosed with both.
Supportive Strategies for Childhood Trauma:
There are many supportive factors that can help prevent risks associated with trauma, benefitting the health of children for the now into the long-term. Parents and teachers, welcoming a trauma informed attitude, can help children develop the resilience to support their overall health using the following few examples:
- Offer structure and consistent family routines (this helps rebuild a sense of safety and security).
- Use firm and consistent limits/consequences rather than shame and harsh punishment when discipline and correction are necessary.
- Plan one-on-one time using playful activities without distractions (Example: Play a game of Jenga, but put away your cell phones and turn off the television in the background).
- Seek education from providers and specialists who can help strengthen your understanding of trauma, and how to support the specific needs of your child.
- Model appropriate ways to show and express your feelings.
- Encourage unstructured play and limit screen time to a task that can be used in moderation.
- Read age appropriate books to children that focus on feelings: Ruby’s Worry/When Sadness Is At Your Door.
- Take time to read and make notes in the following book for parents/significant caregivers: The Whole-Brain Child.
Supportive Strategies for ADHD in Children:
There are many modalities that can support children with ADHD. Most evidence based treatments include pharmacology, parent coaching, and CBT (Cognitive Behavioral Therapy). Parents are a crucial factor in successful treatment outcomes. Here are few strategies below to support parents and significant caregivers:
- Utilize visual aids with clear and concise language.
- Build onto their esteem by noticing their efforts and encouraging them through their struggles.
- Use scaffolding as a tool.
- Welcome an ADHD lens (seek education to help take the perspective of the child).
- Consider consulting with a Child Psychiatrist if curious about the use of medication.
- Work with an ADHD specialist experienced in working with other diagnoses.
- Spend uninterrupted time with your child to increase your knowledge of their needs and support the relationship.
- Read books to support their understanding of the brain functioning and their feelings to appropriately communicate their needs: I Can’t Keep Still & Shelley the Hyperactive Turtle.
- Read parenting books about ADHD: Taking Charge of ADHD & Smart but Scattered.
The benefit of selecting an ADHD specialist and trauma informed provider?
Children receive the most effective care when providers use a developmental focus throughout their approach. It often benefits the child to welcome a collaborative team of providers, who specialize in ADHD and trauma, due to the complexities of child development. This means that a child may participate in play therapy to work through their experience of trauma while also participating in group therapy, or separate service of care, for support through concerns under ADHD. Children may also be referred to tutoring, an occupational therapist, speech-language pathologist, psychological testing, or to their pediatrician. There is strength in taking this holistic approach where trusted referred providers communicate about each area they are focused on, and share clinical observations to keep each other aware of the child’s symptoms. This encouraging way for providers to work together is what helps parents receive the best support for their child while decreasing the chance for misdiagnosis. When providers have the training to work together, progress occurs more quickly and the entire support system receives a greater understanding of the child.
About the Authors:
Taylor Hart (formerly known as Taylor Quick) — Taylor owns The Empathy Nest, PLLC where she provides individual play therapy and talk therapy to children ages 2-12 years old along with services specific to parents/significant caregivers.
Alyse Bone– Alyse is a therapist that currently works primarily with ADHD, ASD, & Anxiety disorders in children ages 3-14, who also have many comorbidities including, trauma, OCD, and depression.
For more information about Alyse please visit her profile: https://dandelionfamilycounseling.com/alyse-bone-lpc/

